New at Nirvana: November
Published:
December 10, 2025
.png)
Published:
December 10, 2025
.png)
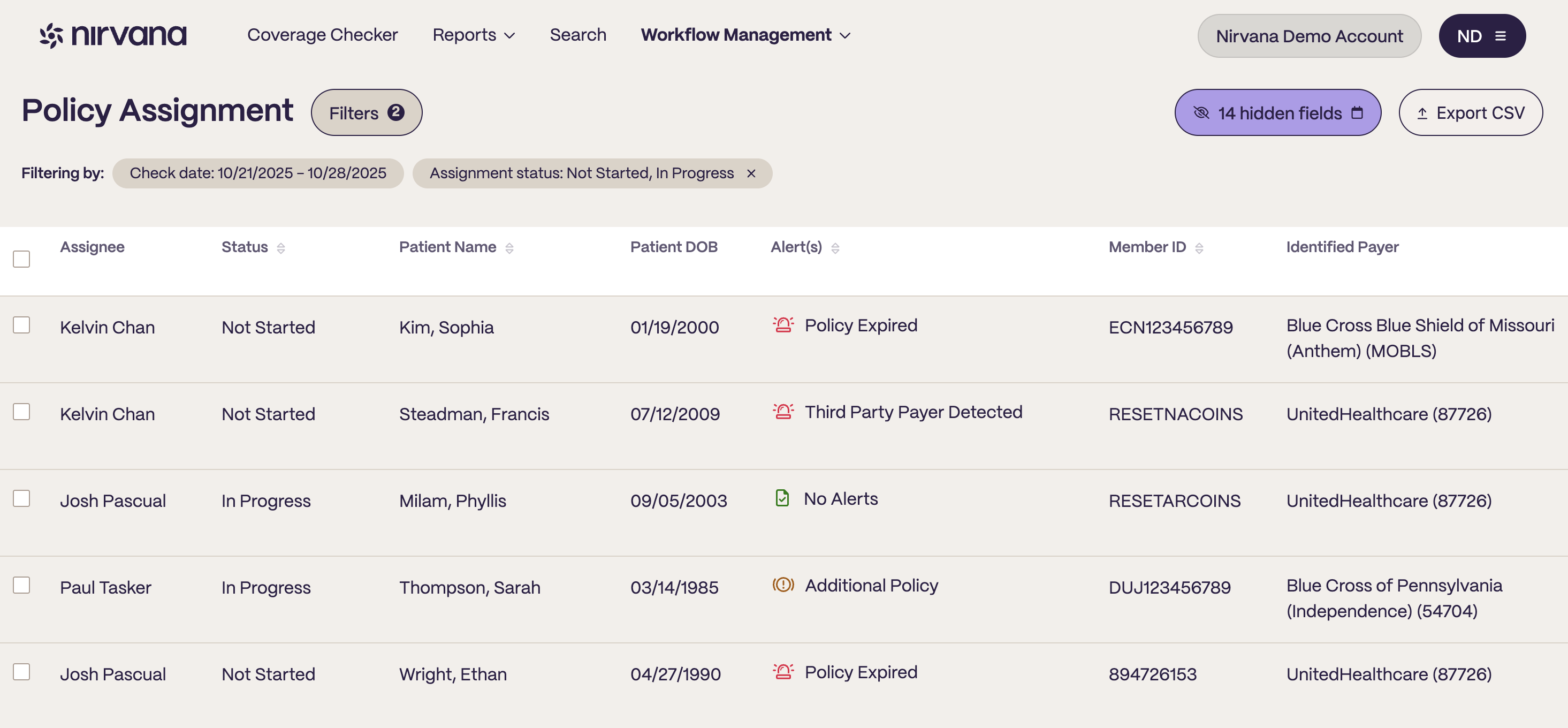
This month we rolled out updates that make eligibility data more consistent across OneVerify and the API–especially for plan classification and reporting–right in time for year-end and benefit resets. We’re also expanding Workflow Management and sharing key payer shifts from our billing team to help you stay ahead.
The new workflow management module is available for free trial in December and January. View, assign, and work all of your checks within one platform. Reduce the need for several sheets, sources, or tabs to manage client's eligibility.
Fill out this form and say you heard about Nirvana on the blog to gain access today!
Magellan has updated its behavioral health criteria, and several major payers are moving away from using Magellan’s as their behavioral health carveout. Many are bringing behavioral health administration in-house, while others are shifting to new behavioral health administrators.
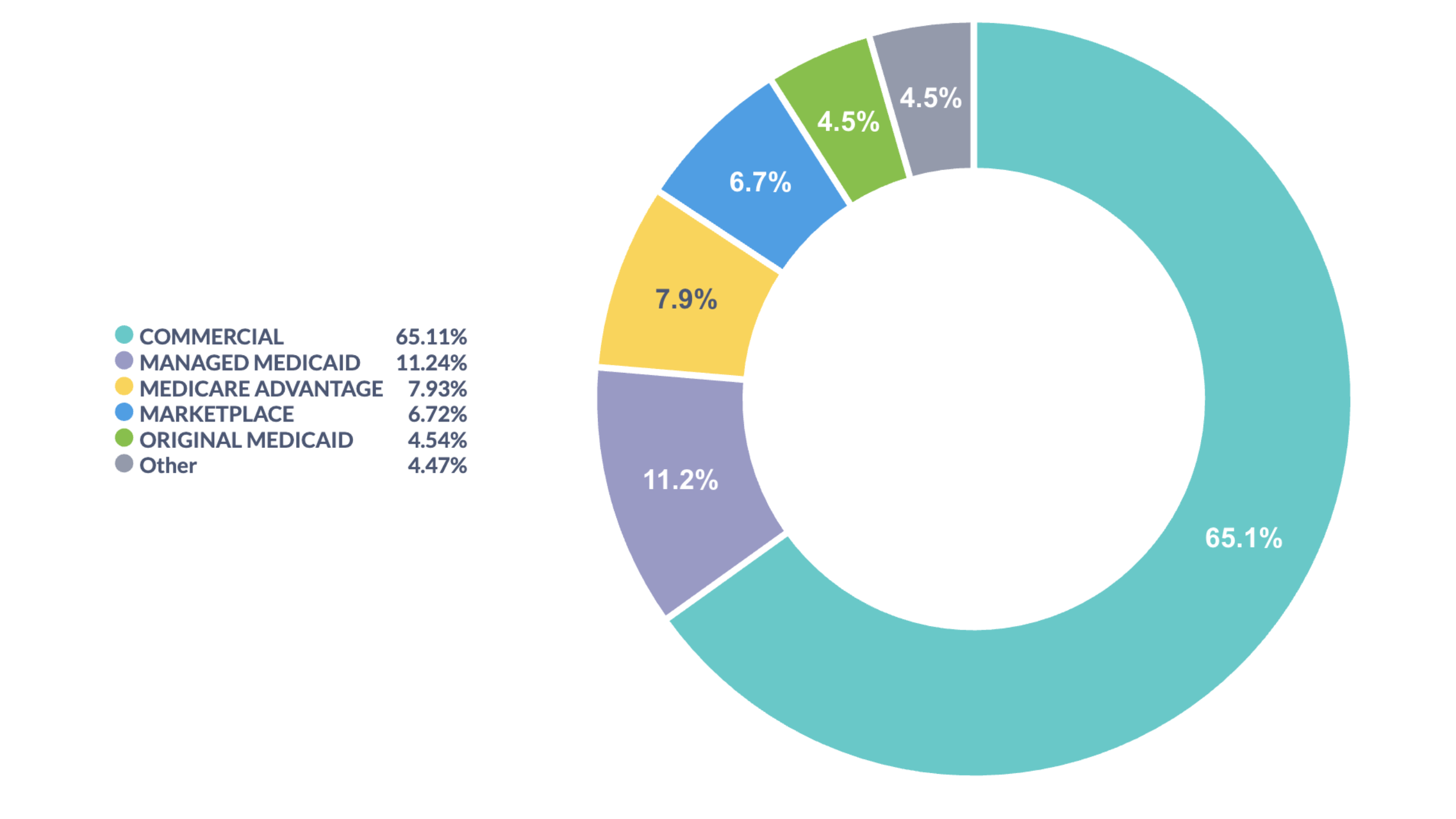
Insights from newly expanded Plan Type Feature:
Annual Benefit Resets are here!
As we finish out the year, and you turn your focus to January verifications and reauthorizations, remember Nirvana is here to help, contact your CSM to ensure you are set up for success. Read more about how we can help on the blog.
Nirvana x CLEAR Partnership
Lowering barriers to intake, streamlining secure, easy, & effective eligibility checks. Read more about how Nirvana is partnering with CLEAR to revolutionize patient check in! Read more on the blog.
Navigating healthcare coverage and costs doesn't have to feel like wandering in the dark.
We're here to light the way.